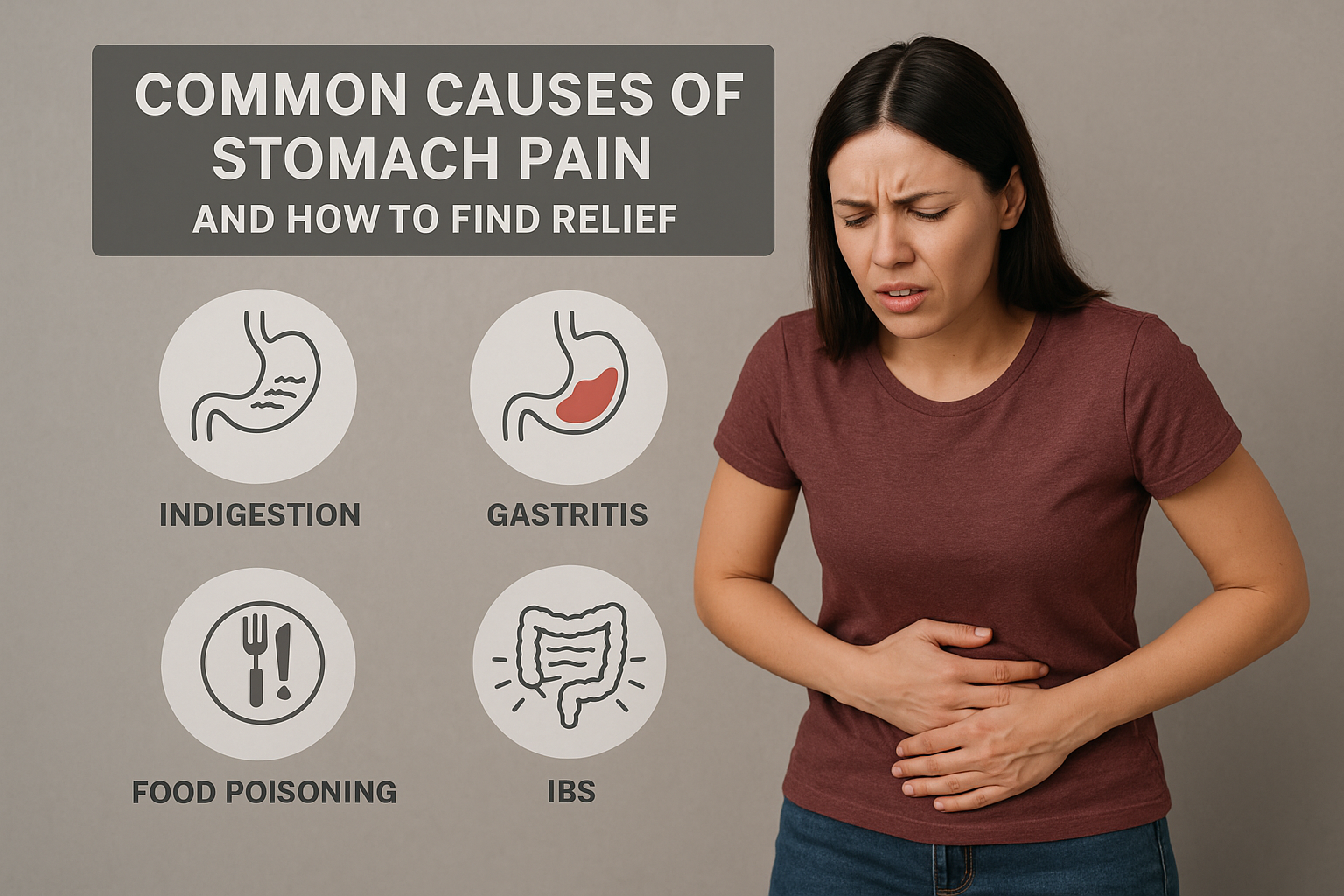
Understanding Stomach Pain
Stomach pain is one of the most frequent digestive complaints. It can range from mild discomfort to severe cramping that affects daily life. The pain may come from issues in the stomach, intestines, liver, gallbladder, or other nearby organs. Identifying the cause early can help you get proper treatment and long-lasting relief.
1. Indigestion – The Most Common Culprit
Indigestion often causes burning pain or fullness in the upper abdomen after meals. It may result from eating too quickly, consuming spicy or fatty foods, or stress. Staying hydrated, avoiding heavy meals before bedtime, and eating smaller portions can help ease symptoms naturally.
2. Acid Reflux and Heartburn
Acid reflux occurs when stomach acid backs up into the esophagus, leading to a burning sensation. It’s often triggered by overeating, caffeine, or lying down after meals. Elevating the head while sleeping and limiting acidic foods can reduce discomfort and improve digestion.
3. Gastritis – Inflammation of the Stomach Lining
Gastritis causes sharp or dull abdominal pain, nausea, and bloating. It may occur due to excessive alcohol, prolonged medication use, or bacterial infections like H. pylori. A balanced diet rich in fiber and probiotics supports healing and strengthens digestive health.
4. Constipation and Bloating
Constipation leads to stomach pressure, bloating, and pain. A lack of fiber, dehydration, and a sedentary lifestyle are common triggers. Increase fiber intake through fruits and vegetables, drink plenty of water, and stay physically active to keep your gut functioning smoothly.
5. Gastroenteritis – Stomach Infection
Gastroenteritis, or stomach flu, is caused by viral or bacterial infection. It leads to vomiting, diarrhea, and abdominal cramps. Rest, hydration, and light meals are essential for recovery. Avoid street food and practice good hygiene to prevent infection.
6. Gallstones and Other Digestive Disorders
Sometimes, stomach pain may stem from gallstones or liver problems. Gallstones cause intense pain after fatty meals. In such cases, professional medical evaluation is vital to prevent complications.
When to See a Doctor
Persistent or severe stomach pain should not be ignored. Symptoms like vomiting blood, unexplained weight loss, or yellowing of the skin need immediate medical care. Visit our KHIMS Hospitals for expert diagnosis and treatment from our experienced gastroenterology team.
Home Remedies and Relief Tips
Eat slowly and chew food thoroughly
Avoid oily, spicy, and processed foods
Drink herbal teas like ginger or peppermint
Maintain regular bowel movements
Manage stress with yoga or meditation
Conclusion
Understanding the common causes of stomach pain helps you take preventive steps for better digestive health. Early treatment and lifestyle changes can bring lasting relief.
For chronic or severe pain, consult the specialists at KHIMS Hospitals for personalized care and advanced treatments.