The human body works as an interconnected system, and gut health plays a crucial role in maintaining overall wellness. Your digestive system does more than process food—it strongly influences immunity, energy levels, and long-term health. Understanding this connection helps in preventing illness and improving quality of life.
The Digestive System: More Than Digestion
The digestive tract breaks down food, absorbs nutrients, and eliminates waste. During this process, it also supports the immune system by acting as a protective barrier against harmful microorganisms. Nearly 70% of immune cells reside in the gut, making digestion central to body defense.
Gut Health and Immunity Connection
A healthy gut contains beneficial bacteria known as gut microbiome, which helps regulate immune responses. These bacteria prevent the growth of pathogens, reduce inflammation, and improve resistance to infections. Poor digestion can weaken immunity and increase disease risk.
Role of Nutrient Absorption
Efficient digestion ensures proper nutrient absorption, supplying vitamins, minerals, and antioxidants required for immune cell production. Deficiencies caused by digestive issues can result in fatigue, frequent infections, and slow recovery.
Digestive Health and Inflammation
An unhealthy gut may lead to chronic inflammation, which negatively impacts overall wellness. Inflammation can contribute to lifestyle disorders, joint pain, and reduced immunity. Balanced digestion helps maintain internal harmony.
How Lifestyle Affects Digestive Wellness
Several daily habits influence digestive performance:
-
Eating a balanced diet rich in fiber
-
Staying hydrated
-
Managing stress levels
-
Getting adequate sleep
-
Limiting processed foods
These practices promote gut balance and immune strength.
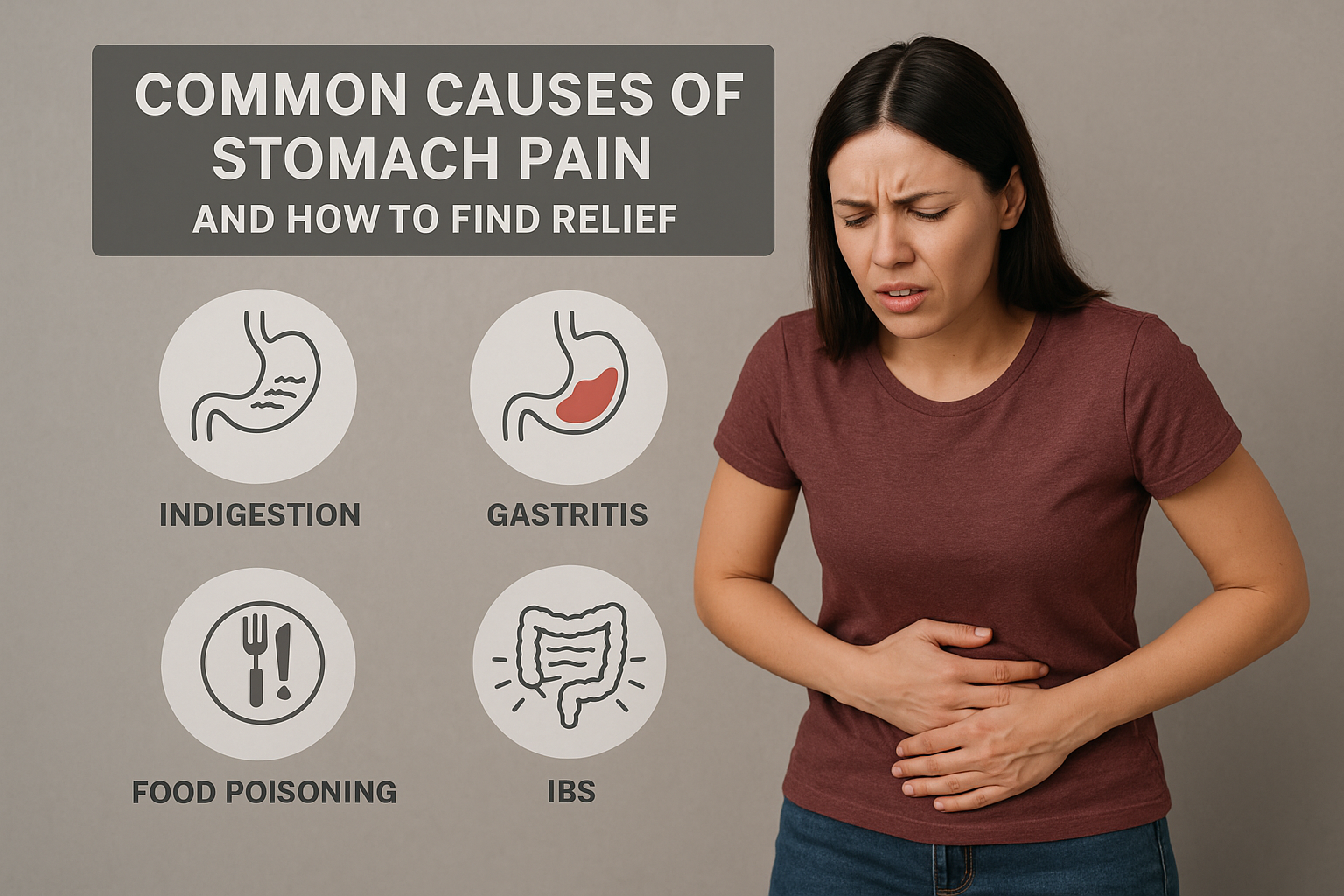
Signs Your Digestive System Needs Attention
Watch for symptoms such as bloating, irregular bowel movements, acidity, or frequent illness. These may indicate poor digestive health affecting immunity.
Supporting Digestive Health Naturally
Simple steps to support digestion include consuming probiotics, regular physical activity, and mindful eating. Medical guidance can further improve gut-related conditions and immune resilience.
When to Consult a Specialist
Persistent digestive problems may require professional evaluation. Expert care ensures accurate diagnosis and effective management to restore wellness. Visit our Khims Hospitals Khammam for comprehensive digestive and immune health support.
Conclusion
Your digestive system is a cornerstone of immunity and wellness. Maintaining digestive balance strengthens the body’s natural defenses and improves daily health.
Prioritizing gut health through proper nutrition and lifestyle choices leads to long-term vitality and disease prevention.