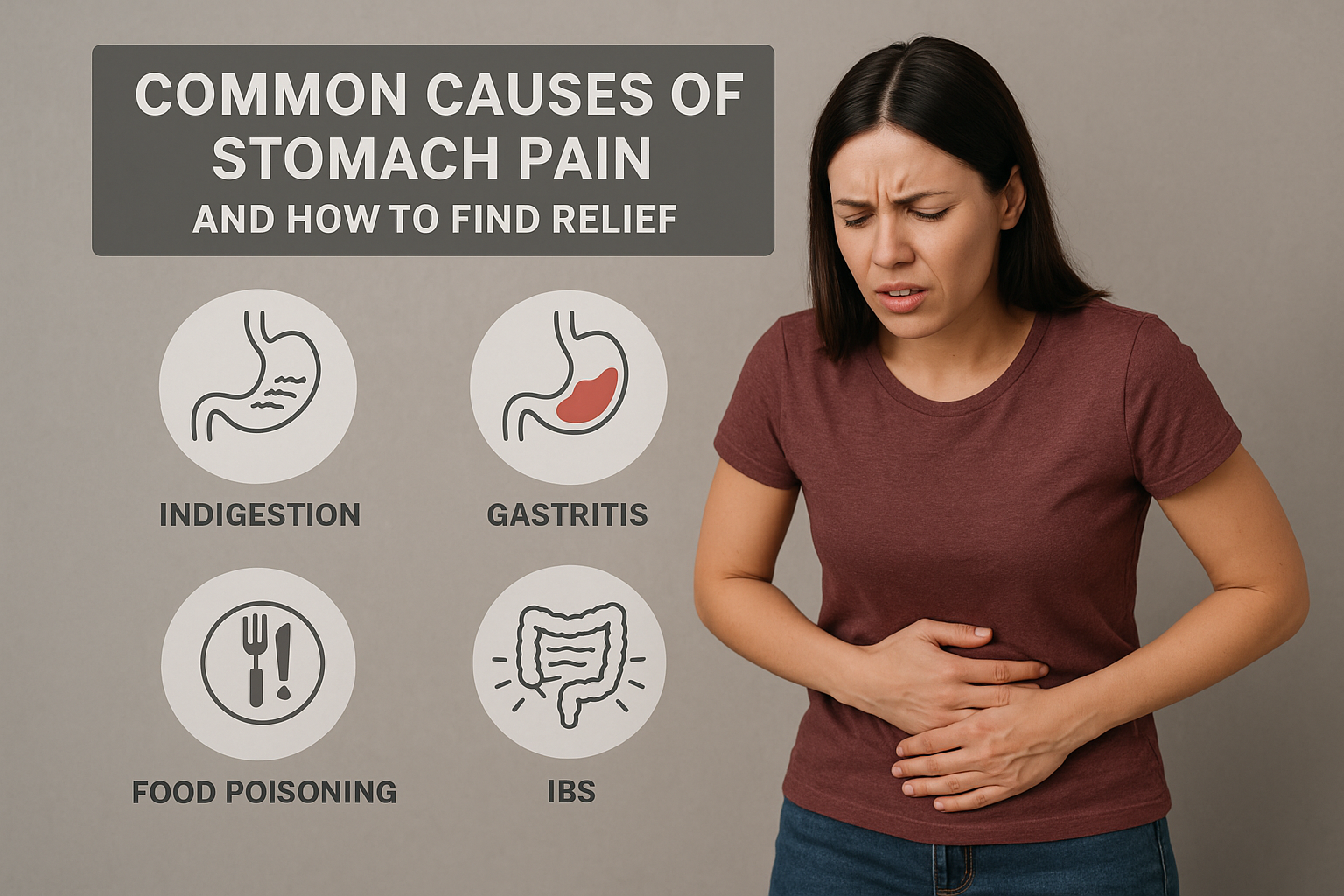
A healthy digestive system plays a major role in overall wellness, immunity, and daily comfort. Many people struggle with bloating, acidity, constipation, or indigestion, which often connect to poor habits. Improving gut function naturally is possible through mindful food choices and small lifestyle changes.
Understanding Gut Health
Your gut contains millions of beneficial bacteria that help digestion, nutrient absorption, and immune strength. An imbalance in this microbiome may lead to issues like irritable bowel, fatigue, or skin problems. Supporting these good bacteria is essential for long-term wellness.
Diet Tips to Boost Gut Health Naturally
1. Add Fiber-Rich Foods
Fiber improves bowel movement and feeds healthy bacteria. Include whole grains, lentils, fruits, vegetables, and seeds to maintain regularity and reduce inflammation.
2. Eat Probiotic-Rich Foods
Probiotics help restore the microbiome. Add curd, kefir, fermented vegetables, and buttermilk. These foods support easy digestion and reduce acidity.
3. Choose Prebiotic Foods
Prebiotics act as fuel for probiotics. Foods like onions, garlic, bananas, asparagus, and oats help maintain balance and support nutrient absorption.
4. Stay Hydrated
Water helps break down food and allows nutrients to travel smoothly through the gut. Adequate hydration prevents constipation and bloating.
5. Reduce Processed Foods
Packaged snacks, sugary drinks, and fast foods harm gut bacteria and trigger inflammation. Replace them with fresh, home-cooked meals for better digestive comfort.
Lifestyle Habits for Better Digestive Health
1. Eat Slowly & Mindfully
Chewing well improves metabolism and reduces reflux. Mindful eating signals the body to release digestive enzymes effectively.
2. Exercise Regularly
Walking, yoga, stretching, and core exercises stimulate bowel movement and reduce gas or constipation.
3. Manage Stress
Chronic stress affects the gut-brain connection. Deep breathing, meditation, and outdoor activities help calm the digestive system.
4. Maintain Good Sleep
Poor sleep disrupts hormones that control digestion. Aim for consistent sleep to support gut recovery and balance.
5. Limit Unnecessary Antibiotics
Overuse of antibiotics harms beneficial bacteria. Take them only with medical guidance to prevent imbalance.
Conclusion
A balanced diet, mindful eating, and regular activity strengthen digestion and overall health. Natural steps like fiber intake, hydration, and probiotics can transform your gut function gently and effectively.
When symptoms persist or disrupt daily life, consult specialists for expert evaluation and holistic treatment. For complete digestive care, visit our KHIMS Hospitals.